Real-time Billing for Health Insurance Board
The Health Insurance Board (HIB) is a social protection initiative by the Government of Nepal, designed to provide citizens with access to quality healthcare services without causing financial hardship. This program actively involves households, communities, and the government in its implementation. By combining prepayment and risk pooling, the Health Insurance program helps protect individuals from falling into poverty due to high medical costs, such as those from accidents or illness. It also advocates for improved healthcare quality and aims to break down barriers to healthcare access, ensuring that underserved and disadvantaged groups can receive the care they need. As part of the effort to achieve Universal Health Coverage, the program plays a crucial role in addressing healthcare inequities.
To ensure comprehensive healthcare coverage, the Health Insurance Board (HIB) offers a range of medical services and medicines through its Health Care Packages. These packages are available to citizens enrolled in the program and are delivered by both private and government health institutions that have received affiliation from the board. The process for claiming insurance differs between private and government healthcare providers, with specific guidelines in place for each.
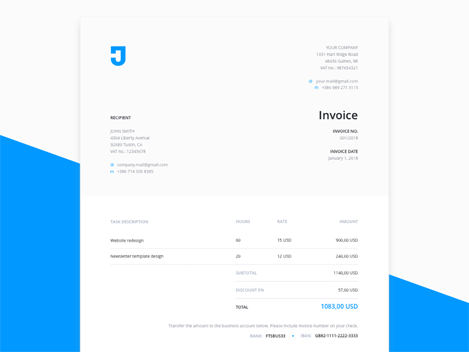
Recently, the Health Insurance Board mandated that all insurance claims must be processed in real time. To facilitate this, they have issued guidelines requiring healthcare providers to implement real-time billing systems for claiming insurance amounts efficiently.
The eHMIS (Electronic Health Management Information System) plays a crucial role in helping health institutions comply with these requirements by offering an integrated health management solution. It includes a real-time billing system that aligns with the Health Insurance Board's guidelines, ensuring seamless synchronization with IMIS (Insurance Management Information System), the official insurance management system of the Government of Nepal.
Key features such as patient enrollment, OPD ticket management, referral management, claim code management, and billing are fully automated and synchronized with IMIS at the click of a button. This automation streamlines daily operations for healthcare professionals, creating a hassle-free environment where tasks are completed efficiently, ensuring timely and accurate insurance claims and reducing administrative burdens.
With its comprehensive integration, eHMIS enhances the efficiency of healthcare services, improving the overall experience for both patients and healthcare providers, while supporting the objectives of the Health Insurance Board for real-time, quality healthcare delivery.
Real-time billing
Real-time billing enables health institutions to seamlessly retrieve client records from the Health Insurance Board database, including available balance details. The system also automates the fetching of prescribed services and medications based on the doctor's prescriptions, streamlining the billing process. This feature allows healthcare personnel to generate prompt and accurate bills, reducing manual errors and increasing efficiency in patient service delivery.
Automated Prescription Card Upload
When submitting claims to the Health Insurance Board, it is mandatory to upload the doctor’s prescription. Our system includes a feature that allows healthcare personnel to upload the prescription, complete with an authorized signature, in just one click. This streamlined process significantly reduces the time and effort involved in manually uploading documents, improving efficiency and accuracy in claim submissions.
See Electronic Health Management Information System (eHMIS)
Digitizing Your Health Institution for a Smarter Future
- Support 9/6
- Cancel anytime